ICU at home: When is it safe to move a patient from the hospital to home?
Medical Equipment
Jan 30, 2026
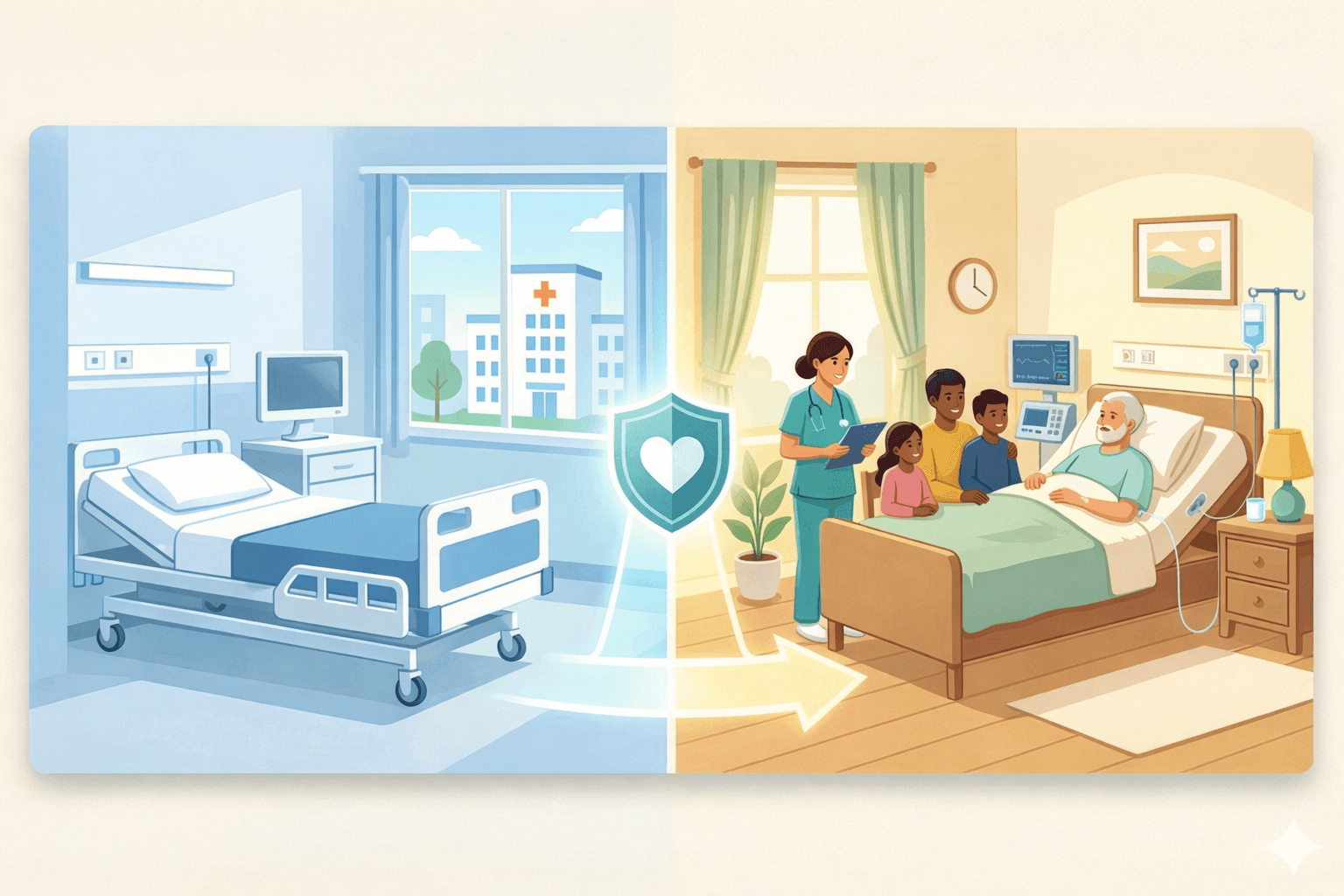
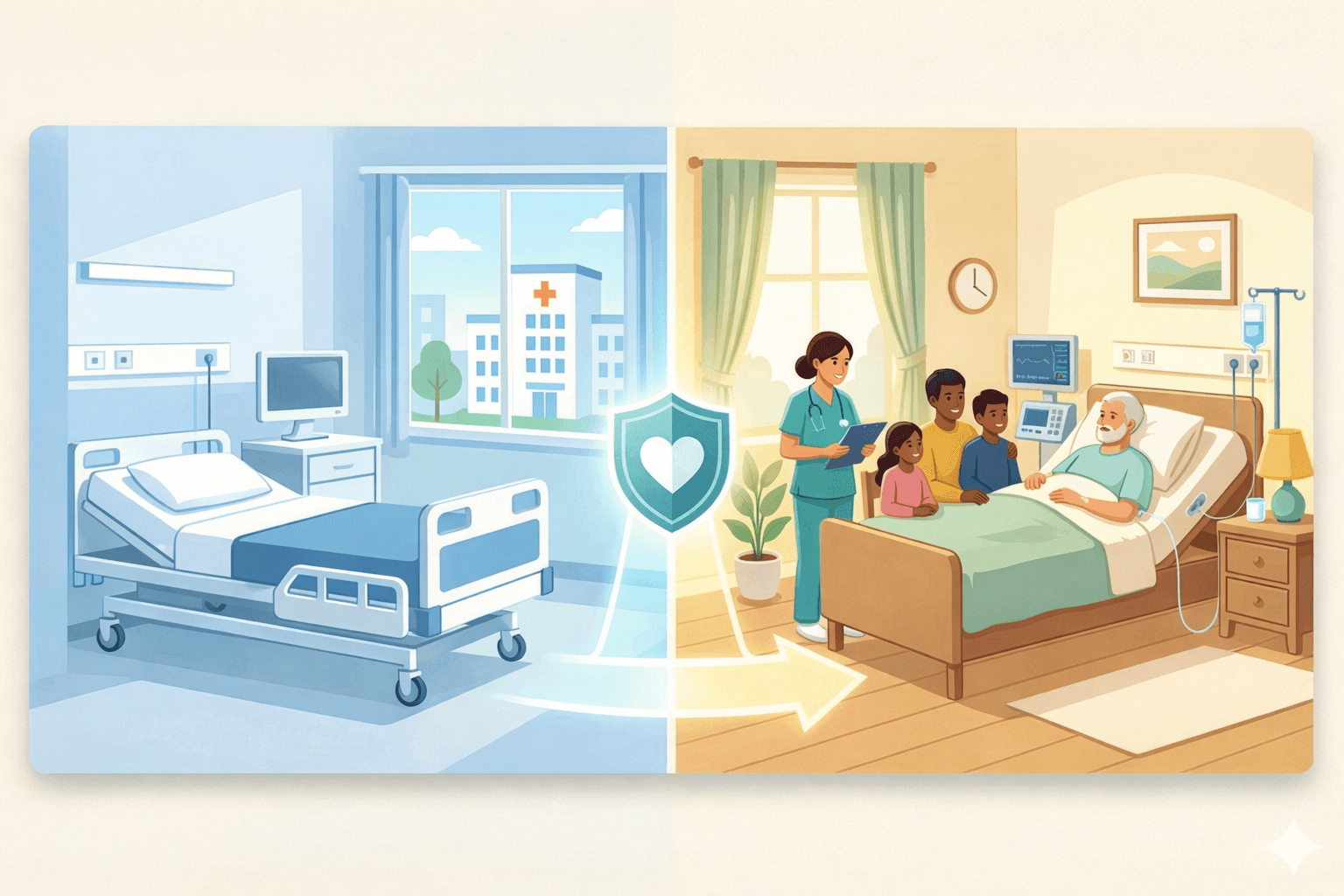
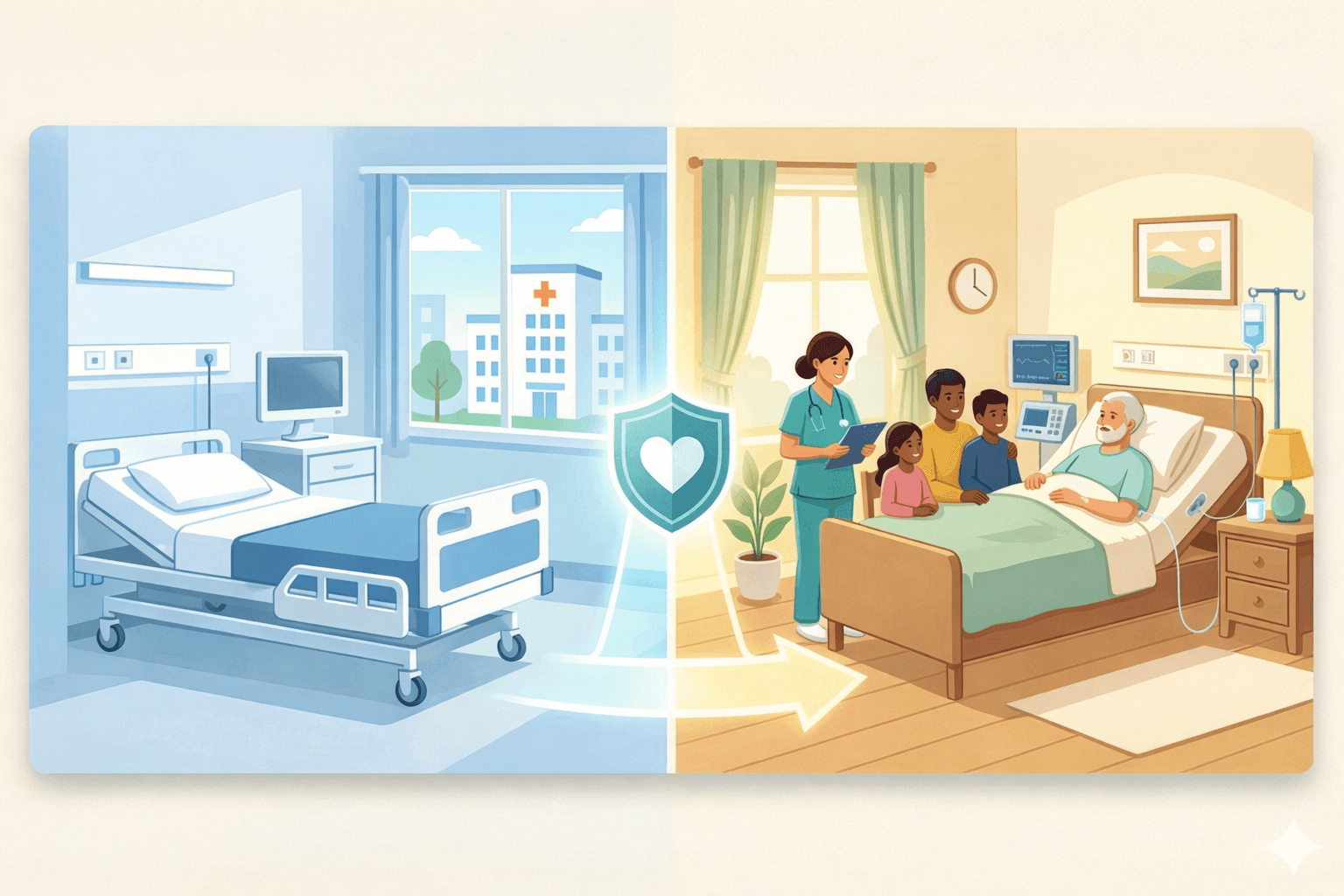
The decision to move a critically ill family member from the hospital ICU to home care feels overwhelming. Questions flood in: Is it safe? Will we have the right equipment? Can nurses provide the same level of care at home? These concerns are valid, but with proper planning and professional support, ICU-level care at home is not only possible but often beneficial for patients and families.
Understanding when this transition makes sense and how to ensure safety requires knowledge of medical criteria, available resources, and realistic expectations.
Let's explore when moving from hospital ICU to home becomes the right choice.
What does ICU at home mean?
ICU at home recreates the critical care environment within the patient's residence. This includes advanced medical equipment, round-the-clock nursing supervision, physician oversight, and emergency protocols, all coordinated to provide hospital-level monitoring and treatment in familiar surroundings.
Modern home ICU setups can support:
Ventilator-dependent patients require breathing assistance.
Continuous vital sign monitoring (heart rate, blood pressure, oxygen levels).
IV medication administration and pain management.
Tracheostomy care and suctioning.
Post-surgical wound management and infection prevention.
Feeding through nasogastric or gastrostomy tubes.
The capability extends beyond basic nursing care to include sophisticated medical interventions that were once possible only in hospital settings.
When is a patient medically stable enough for home ICU?
Not every ICU patient can safely transition home. Medical stability forms the foundation of this decision. Physicians evaluate several factors before approving home-based critical care.
Key criteria for ICU discharge to home:
Vital signs have stabilised and returned to near-baseline levels.
The acute medical crisis has resolved, though ongoing intensive monitoring remains necessary.
No immediate need for emergency surgical intervention or specialised hospital procedures.
Respiratory status is manageable with available home ventilation equipment.
Infection markers are controlled, and antibiotic regimens can continue at home.
Family and caregivers are prepared to participate in care routines.
According to India's ICU admission and discharge guidelines, patients should be discharged when physiological parameters return to near normal, and the acute illness has reasonably resolved. This doesn't mean complete recovery; it means stability that can be maintained with appropriate home-based support.
What conditions can be managed with ICU at home?
Certain medical situations particularly benefit from transitioning to home-based intensive care after initial hospital stabilisation.
Condition | How ICU at home helps |
Prolonged ventilator dependence | Long-term breathing support with home ventilators, regular suctioning, monitoring oxygen saturation, and preventing ventilator-associated complications. |
Post-stroke recovery | Intensive rehabilitation, preventing secondary complications, managing medications, monitoring neurological status, and supporting family involvement. |
Advanced heart failure | Continuous cardiac monitoring, medication management, fluid balance tracking, oxygen therapy, and symptom control. |
Chronic respiratory disease (COPD) | Oxygen therapy management, breathing exercises, medication nebulisation, preventing exacerbations, and infection monitoring. |
Cancer care/palliative support | Pain management, symptom control, maintaining dignity, family presence, comfort-focused intensive care. |
Post-surgical complications | Wound care, infection prevention, pain control, monitoring recovery progress, and preventing hospital-acquired infections. |
How does home ICU compare financially to hospital care?
The cost difference between hospital ICU and home-based intensive care is substantial. In private hospitals across India, ICU charges range from ₹15,000 to ₹30,000 per day, with premium facilities charging even more. These costs exclude medications, diagnostic tests, specialist consultations, and consumables that appear as separate line items on bills.
Home ICU services operate differently. The typical cost ranges from ₹7,000 to ₹10,000 per day, covering nursing care, equipment rental, basic monitoring, and coordination. For families facing extended critical care needs, this represents significant savings whilst maintaining clinical quality.
Consider a patient requiring ventilator support for three months. Hospital ICU costs could exceed ₹20 lakhs, creating enormous financial pressure. Home ICU for the same period might cost ₹7-9 lakhs, less than half, whilst providing dedicated attention and family involvement impossible in hospital settings.
What medical equipment is needed for a home ICU setup?
Creating a safe home ICU environment requires specific equipment that matches the patient's medical needs. Professional medical equipment providers arrange everything necessary for critical care at home.
Essential equipment typically includes:
Ventilator or BiPAP machine: Provides breathing support with adjustable settings based on patient requirements.
Oxygen concentrator or cylinder: Ensures a continuous oxygen supply with backup systems for emergencies.
Cardiac monitor: Tracks heart rate, rhythm, and detects abnormalities requiring immediate intervention.
Pulse oximeter: Monitors oxygen saturation continuously, alerting caregivers to concerning changes.
Hospital bed: Electric ICU beds with adjustable positions, side rails, and pressure-relief features.
Suction machine: Removes secretions from airways, essential for tracheostomy or ventilator patients.
IV stands and pumps: Delivers medications at precise rates, manages fluid administration.
Nebuliser: Administers respiratory medications directly to the lungs.
All equipment comes with installation, training, and maintenance support. Backup power arrangements ensure uninterrupted operation during electricity failures, critical for life-support devices.
Can nurses provide the same level of care as a hospital ICU?
The nursing care provided at home for ICU patients follows the same clinical protocols used in hospitals, often with superior personalisation and attention. Critical care nurses assigned to home ICU cases bring specialised training in managing complex medical situations.
These nurses handle:
Ventilator management, adjusting settings based on patient response.
Tracheostomy care, suctioning, and preventing infections.
IV medication administration, including high-risk drugs.
Wound dressing and sterile technique maintenance.
Vital sign monitoring and identifying concerning trends.
Emergency response protocols and physician coordination.
Family education about care routines and warning signs.
Unlike hospital settings where nurses manage multiple patients simultaneously, the home ICU provides dedicated one-to-one nursing attention. This focused care often catches subtle changes earlier, prevents complications more effectively, and responds to patient needs more immediately. As discussed in our guide on home nursing care for chronic illness, this personalised approach significantly improves patient outcomes.
What role does family play in home ICU care?
Family involvement transforms from limited visiting hours to active participation in the care process. This doesn't mean families shoulder the medical burden; professional nurses handle technical aspects. Instead, families provide emotional support, maintain normalcy, and assist with daily comfort measures.
Effective family participation includes:
Learning to recognise warning signs that require a nurse's attention.
Assisting with feeding, gentle repositioning, and personal hygiene.
Maintaining familiar routines that provide psychological comfort.
Communicating patient preferences and concerns to care teams.
Making medical decisions in consultation with physicians.
Professional nurses educate families throughout the process, building confidence without creating dependence. This partnership approach ensures patients receive both expert medical care and the emotional support that only family can provide.
What are the signs that hospital readmission becomes necessary?
Despite best efforts, some situations require returning to hospital facilities. Recognising these early allows for smooth transitions rather than crisis admissions.
Warning signs requiring hospital care:
Sudden deterioration in consciousness or responsiveness.
Persistent high fever uncontrolled by medications.
Severe breathing difficulty despite ventilator adjustment.
Chest pain or cardiac rhythm changes.
Uncontrolled bleeding or surgical wound complications.
Seizures or neurological changes.
Equipment failures that cannot be immediately resolved.
Professional home healthcare teams monitor these indicators continuously and coordinate hospital readmission when necessary. The goal isn't avoiding hospitals entirely, it's using them appropriately for acute interventions whilst providing superior ongoing care at home.
How do you choose the right home ICU provider?
Selecting a qualified home ICU service requires evaluating several critical factors that determine safety and quality.
Essential qualities to verify:
Critical care nurses with ICU experience and proper certification.
24/7 availability, including nights, weekends, and holidays.
Comprehensive equipment inventory, including backup systems.
Established relationships with hospitals for emergency admissions.
Transparent pricing without hidden equipment or supply charges.
Physician network for ongoing medical supervision.
Clear communication protocols keep families informed.
Proven track record in managing similar patient conditions.
Ask specific questions about nurse qualifications, emergency protocols, equipment maintenance, and physician involvement. Request references from families who've used their services for comparable situations.
Making the transition from hospital to home ICU
The actual move from hospital to home requires careful planning and coordination. Professional home ICU providers manage this transition systematically to ensure patient safety throughout.
Transition steps include:
Medical assessment: Physician reviews confirm patient stability and appropriate discharge criteria.
Home preparation: Equipment installation, room setup, and safety modifications completed before patient arrival.
Care team coordination: Nurses receive a detailed handover from hospital staff about treatment plans and patient needs.
Family education: Training sessions prepare families for what to expect and how to support care routines.
Trial period: Initial days include extra monitoring to ensure all systems function properly and address any adjustment challenges.
Most transitions occur smoothly when properly planned. Patients often show immediate improvement once settled in familiar surroundings with dedicated nursing attention.
Making the transition to ICU care at home
ICU care at home is about continuity, not compromise. For patients who are medically stable but still need close monitoring, it allows intensive care to continue in familiar surroundings rather than a hospital ICU.
With doctor-led oversight, trained critical care nurses, and appropriate medical equipment, patients can receive safe, structured ICU-level care at home while remaining close to family. This approach often supports comfort, emotional well-being, and smoother long-term recovery.
Heka Health provides ICU at home services designed around individual medical needs, with personalised care plans, continuous monitoring, and coordinated clinical support. The focus remains on safety, dignity, and maintaining quality of life beyond the hospital setting.
Reach out to our team to discuss your requirements. We’ll take the time to understand the patient’s condition and then guide you through the appropriate next steps for ICU care at home.
Your well-being
is our priority.
Together, let's navigate every step
with care and compassion.

Your well-being
is our priority.
Together, let's navigate every step
with care and compassion.

Your well-being
is our priority.
Together, let's navigate every step
with care and compassion.
